Daniel E Freedberg, MD
On the web

Overview
I am a a clinical and translational investigator focused on the relationship between the gastrointestinal microbiome and infections, both enteric and non-enteric.
Dr. Freedberg graduated from Harvard Medical School and completed his residency and fellowship training at Columbia University. He received a Master's degree in biostatistics from Columbia's Mailman School of Public Health. Dr. Freedberg's research focuses on the use of acid suppression medications, Clostridium difficile infection, and the gastrointestinal microbiome. Current projects include studies of how acid suppression medications alter the colonic microbiome and of how alterations in the gastrointestinal flora predispose patients to Clostridium difficile and other infections during periods of critical illness. His research is funded by the National Institutes of Health and the American Gastroenterological Association.
Dr. Freedberg is a clinical and translational investigator focused on the relationship between the gastrointestinal microbiome and infections, both enteric and non-enteric. He is a graduate of Harvard Medical School and the Mailman School of Public Health and trained in medicine and gastroenterology at Columbia University Medical Center. He is the past recipient of an American Gastroenterological Association (AGA) Research Scholar Award and has received funding from the NIH/NIDDK, Irving Institute (Columbia's CTSA), and the Department of Defense. His work has been published in leading journals across disciplines: Gastroenterology, Clinical Infectious Disease, Intensive Care Medicine, JAMA Internal Medicine, and Nature. Currently, he focuses on the gastrointestinal microbiome in the intensive care unit (ICU). He has built large ICU cohorts containing longitudinal clinical data, serial rectal swabs, other biosamples, and clinical outcomes data. These samples and data have been collected to understand the dynamic changes that take place within the gastrointestinal microbiome during critical illness and to ask how these changes may impact risk for ICU-acquired infections. His past studies in this area show the importance of colonizing pathogens such as C. difficile and vancomycin-resistant Enterococcus (VRE) as determinants not only of the patient's own health but of outcomes for patients who share the same hospital environment. Ongoing research tests interventions seeking to improve the resistance of the native gut microbiota against pathogens, with a goal of preventing colonization and downstream infection in the ICU.
Areas of Expertise / Conditions Treated
- Barrett's Esophagus
- Celiac Disease
- Clostridioides Difficile (C. diff) Colitis
- Colon Cancer
- Colon Cancer Screening
- Colonoscopy
- Crohn's Disease
- Cyclic Vomiting Syndrome (CVS)
- Digestive System Disorder
- Eosinophilic Esophagitis
- Esophageal Disease
- Esophageal Motility Disorder
- Esophageal Stricture
- Fecal Microbiota Transplantation (FMT)
- Gastric Outlet Obstruction
- Gastrointestinal Cancer
- Gastrointestinal Disease
- Gastrointestinal Motility
- General Gastroenterology
- Inflammatory Bowel Disease (IBD)
- Positive Cologuard
- Virtual Colonoscopy
- Zenker's Diverticulum
Academic Appointments
- Assistant Professor Medicine and Epidemiology
Hospital Affiliations
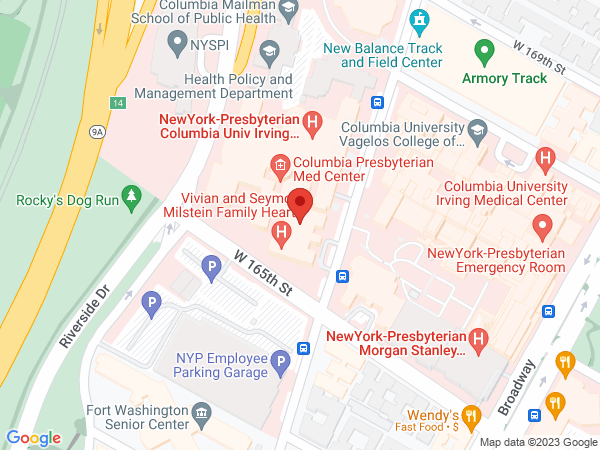
- NewYork-Presbyterian / Columbia University Irving Medical Center
- NewYork-Presbyterian Westchester
Gender
- Male
Schedule an Appointment
Virtual Visits/Telehealth
Virtual Visits allow you to connect with your provider from the comfort, convenience, and safety of your own home.
Phone Appointments
Connect Patient Portal
For existing patients, login to make an appointment, view documentation or contact your care provider.
Location(s)
Insurance Accepted
AETNA
- Aetna Signature Administrators
- EPO
- HMO
- Medicare Managed Care
- NY Signature
- POS
- PPO
- Student Health
Affinity Health Plan
- Essential Plan
- Medicaid Managed Care
Amida Care
- Special Needs
CIGNA
- EPO
- Great West (National)
- HMO
- Medicare Managed Care
- POS
- PPO
Emblem/GHI
- Medicare Managed Care
- PPO
Emblem/HIP
- ConnectiCare
- EPO
- Essential Plan
- HMO
- Medicaid Managed Care
- Medicare Managed Care
- POS
- PPO
- Select Care (Exchange)
- Vytra
Empire Blue Cross/Blue Shield
- EPO
- HMO
- Medicare Managed Care
- PPO
Empire Blue Cross Blue Shield HealthPlus
- Child/Family Health Plus
- Essential Plan
- Medicaid Managed Care
Fidelis Care
- Child/Family Health Plus
- Essential Plan
- Medicaid Managed Care
- Medicare Managed Care
Healthfirst
- Child/Family Health Plus
- Leaf (Exchange)
- Medicaid Managed Care
- Medicare Managed Care
Local 1199
- Local 1199
- NYP Employee Plan
MagnaCare (National)
- MagnaCare
Medicare
- Railroad
- Traditional Medicare
Multiplan
- Multiplan
MVP Health Care
- Child/Family Health Plus
- Essential Plan
- HMO
- Medicaid Managed Care
RiverSpring
- Special Needs
UnitedHealthcare
- Compass (Exchange)
- Empire Plan
- HMO
- Medicaid (Community Plan)
- Medicare Managed Care
- Oxford Freedom
- Oxford HMO
- Oxford Liberty
- POS
- PPO
VNSNY CHOICE
- Medicare Managed Care
- SelectHealth
- Special Needs
WellCare
- Medicaid Managed Care
- Medicare Managed Care
World Trade Center Health Plan
- World Trade Center Health Plan
Credentials & Experience
Education & Training
- MD, 2008 Harvard Medical School
- MD, 2008 Harvard Medical School
- MS, 2014 Columbia University, Mailman School of Public Health
- Residency: NewYork-Presbyterian Hospital/Columbia University Medical Center
- Fellowship: NewYork-Presbyterian Hospital/Columbia University Medical Center
Board Certifications
- Gastroenterology
- Internal Medicine
Honors & Awards
2019 Selected as an AGA Future Leader
2017 Ewig Clinical Scholar Award
2017 John N. Loeb annual lecturer
2016 IDSA/SHEA top 10 most influential article
Research
I am a a clinical and translational investigator focused on the relationship between the gastrointestinal microbiome and infections, both enteric and non-enteric.
I am a clinical and translational investigator focused on enteric infections and the gastrointestinal microbiome in the setting of critical illness. I have experience in molecular laboratory research, clinical training as a physician, a dual appointment in Medicine and Epidemiology, and am the recipient of several grants supporting ICU-based human subjects research focused around enteric colonization in the ICU. With funding from the NIH, the American Gastroenterological Association (AGA), and the Department of Defense, I have built large ICU patient cohorts containing longitudinal clinical data, serial rectal swabs, whole stools, and other bio-samples. These data have allowed us to interrogate the dynamic changes that take place within the gastrointestinal microbiome during critical illness and to ask how these changes may impact risk for ICU-acquired infections. Our preliminary studies show that colonizing enteric organisms such as vancomycin-resistant Enterococcus (VRE) are important determinants of patients’ subsequent risk for infection. We have also found that colonizing enteric organisms can change health outcomes for patients who share the same hospital environment, even if these neighboring patients are not themselves colonized. The normal native microbiota resists colonization with VRE, C. difficile, and similar multidrug-resistant or antibiotic-associated organisms, and a major focus of our current work is how to augment enteric colonization resistance in the face of ICU antibiotics.
Research Interests
- Biostatistical Methods
- Environmental Health
- Food Policy and Obesity
- Infectious Diseases
Selected Publications
-
Wang Y, Schluger A, Li J, Gomez-Simmonds A. Salmasian H, Freedberg D. Does addition of intravenous metronidazole to oral vancomycin improve outcomes in clostridioides difficile infection? Clin Infect Dis. 2019 pii: ciz1115. doi: 10.1093/cid/ciz1115. PMID: 31714955
-
Freedberg DE, Zhou MJ, Cohen ME, Annavajhala MK, Khan S, Moscoso DI, Brooks C, Whittier S, Chong DH, Uhlemann AC, Abrams JA. Pathogen colonization of the gastrointestinal microbiome at intensive care unit admission and risk for subsequent death or infection. Intensive Care Med. 2018; 44(8):1203-1211. PMID: 29936583
-
Seeley JJ, Baker RG, Mohamed G, Bruns T, Hayden MS, Deshmukh SD, Freedberg DE, Ghosh S. Induction of innate immune memory via microRNA targeting of chromatin remodelling factors. Nature. 2018; 559(7712):114-119. PMID: 29950719
For a complete list of publications, please visit PubMed.gov